6 Best Practices in Medical Billing and Collection
Just like any other commerce, profit is the lifeblood of a healthcare business. However, the lack of proper medical billing and coding processes can impact revenue collection negatively.
Studies have shown that coding errors can cause substantial profit losses since these mistakes often lead to denials that delay payment and affect cash flow. For example, a mismatched code can result in upcoding or undercoding. Missing codes can also cause claims to be rejected.
In this article, we’ll discuss the importance of a proper medical billing process for healthcare businesses and six best practices to make medical billing and collection easier. Essentially, these best practices can help you stabilize your cash flow so you can continue providing quality healthcare to your patients.
The Cost of Not Having a Proper Medical Billing Process
According to studies, losses attributed to the lack of a medical billing process can cost up to billions. In the U. S., an estimated $125 billion is left uncollected each year because of poor medical billing practices. In one study, 42% of claims incorrectly coded resulted in $6.7 billion improper Medicare payments.
Another study found coding errors in 89.4% of the selected patient medical records. Accordingly, the potential loss of income due to such inaccuracies was pegged at about $160,000. Still, more money is being lost due to inefficient medical billing practices.
Now that you know the consequences of inefficient medical billing, let’s look at some best practices you can apply to your healthcare business to take control of your medical billing process.
Best Practices in Medical Billing and Collection
1. Verify insurance eligibility at the time of service.
Validating the patient’s insurance eligibility with every visit helps avoid claim denials. Insurance coverage differs between companies, individuals, and plans. If the patient’s insurance does not cover the service to be rendered, it is important to let them know that they will have to cover the entirety of the bill.
Checking for errors in a claim on the spot can also minimize the occurrence of rejections. Keeping in touch with a representative of the payer is vital, as they can help clarify problems with the claim and provide information on current claims as they are processed. This can help expedite the claim editing process and minimize resubmission times.
While the claims submission process demands time and labor, this concern can be addressed by medical billing and coding companies, which employ specialists who guarantee that claims are filed correctly. With an efficient submission system, the shortest collection period possible can be realized, preventing any bottlenecks on your cash flow.
2. Get the patient involved in the process.
The information you collect can be more accurate if you let patients actively participate in the billing process. This lessens instances of coding errors, helping you establish a good rapport with patients.
Medical billing outsourcing services are ideal for this area since they are built on specialized healthcare methods and procedures that facilitate a more efficient collection system.
It also helps to explain the cost breakdown to patients before rendering any services. With this, they will have an understanding of their financial responsibility. At the same time, it creates transparency and trust between your staff and the patient, which can help avoid erroneous billing later.

3. Get the details right.
If claims are not filed correctly, they will not be paid. Thus, taking the time to ensure that all codes are correct and requirements have been met is key to minimizing errors.
While national standards for electronic healthcare transactions are in place, errors can still occur. The most common mistakes, such as incorrect, mismatched, or missing codes, are often a concern.
Partnering with a medical billing outsourcing company is an ideal solution. For healthcare businesses, it allows them to focus on what they do best—providing healthcare to patients—while leaving the details to trained medical coders who are less likely to make crucial errors.
Experts suggest that engaging in regular claims scrubbing can also reduce coding errors, as the process helps identify and perform corrections for errors in billing codes. As a result, it generates cleaner claims, which in turn minimizes denials and improves payer communication.
4. Invest in staff training.
Training allows you to improve and strengthen employee skills, which results in increased efficiency and better work performance. After coming up with a standardized billing process, training your staff members to implement it becomes essential.
Collaborating with a team of medical billing and coding specialists can be helpful in this aspect since they are usually on top of the most current regulations, enabling them to meet the changing demands of serving hospital-based specialty practices.
Essentially, an efficient billing system depends on a well-trained staff who have the ability and necessary skills and tools to check patient eligibility and benefits and collect patient balances.
5. Make time for regular follow-ups.
Once the bill is sent, there should be a follow-up process in place. This should include calling insurance companies to check claim status so that issues can be addressed on time. Verifying with the patients about their payment options can also help create transparency, facilitating the payment process.
Generating monthly accounts receivable reports by using a software management information system is another way to streamline the follow-up process, as this helps identify accounts that are past due. Usually, medical billing and coding companies provide assistance in this area since they are equipped with the proper tools needed for the task.
6. Consider outsourcing your medical billing and collection needs.
Due to the costly time and labor involved in submitting claims, many healthcare providers still find themselves lagging. In dealing with this, some have outsourced their medical billing and coding to third-party specialists, as it proves to be an effective way to increase revenue while cutting labor costs.
For one thing, medical billing companies are compliant with the most recent health care laws, making them abreast with the current guidelines in the industry.
Healthcare billing enterprises also utilize a revenue cycle management (RCM), which strategically addresses coding concerns. Other RCM challenges also fall under the expertise of these companies since they specialize in the coding and collection processes.
Conclusion
If you find yourself dropping behind or failing to stay on top of current regulations, you may want to consider outsourcing third-party specialists. Medical billing and coding companies have greater efficiency and attention to detail because of their specialized tasks, ensuring that claims are filed correctly and denied claims are resubmitted properly. This ultimately results in operational excellence.
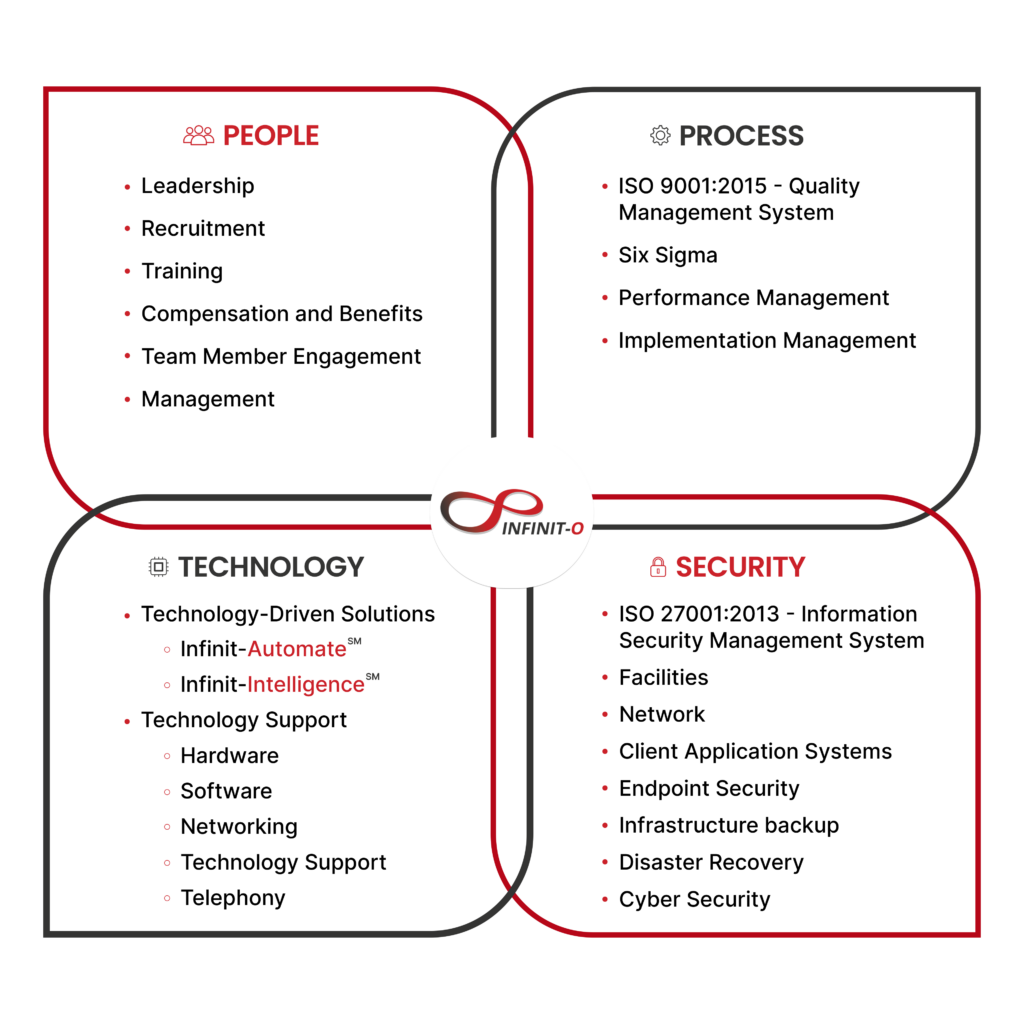
When it comes to outsourcing medical billing teams, Infinit-O is a top choice for a healthcare outsourcing provider that offers the following benefits:
- Access to certified medical billers
- Cost savings of up to 70%
- Operational excellence
- ISO-certified in information security and quality management (ISO 27001 and 9001)
- Compliant with privacy laws, such as the GDPR, HIPAA, and the Data Privacy Act of 2012
In addition, Infinit-O has a Net Promoter Score (NPS) of 71, which means that it prioritizes client experience and that customers are more likely to recommend it to others. The score also reflects high customer loyalty and satisfaction rating regarding the company’s services.
Let’s work together to build an efficient medical billing process for your healthcare business.
Start small. Exceed expectations. Think infinitely. Think Infinit-O.







This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.