How a Great RCM Team Improves Clinical Documentation
Clinical documentation is an integral part of patient care. With this, a thorough record of the diagnoses made, symptoms observed, and services provided on a patient is created. In short, this is the foundation of a patient’s medical record. When done precisely, it can be used to submit valid claims for reimbursement, but on the flip side, incomplete and inaccurate documentation on patient care or those that do not support the billing codes may result in denial of claims.
To prevent this from happening, Clinical Documentation Improvement (CDI) must be done to ensure that the events of the patient encounter are captured accurately and the electronic health record (EHR) properly reflects the services that were provided.
Ultimately, it is focused on two things:
1. improving the quality and value of clinical documentation to improve patient care
2. maximizing revenue and reducing medical coding and billing errors
When it comes to conducting CDI, it is beneficial to have a dedicated team of Revenue Cycle Management (RCM) specialists on your operations.
This team consists of:
- Medical coders and billers – who have the role of translating a patient encounter into the languages used from claims submission and reimbursement
- Clinical documentation specialists – who review medical records, ensure medical codes have been inputted correctly
Below are 4 reasons how a great team of RCM experts improves your Clinical Documentation process:
- They have expert knowledge on ICD-10 and CPT coding
Diagnosis codes play an important part in clinical documentation. These are used to describe a patient’s condition or injury, as well as social determinants of health and other patient characteristics. To capture diagnosis codes for billing purposes, the industry uses the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10).
Procedure codes, on the other hand, complement diagnosis codes by indicating what providers did during an encounter. The two main procedure coding systems are the Current Procedural Terminology (CPT) codes and the Healthcare Common Procedure Coding System (HCPCS).
The Center for Medicare and Medicaid Services (CMS) determines the ICD-10 coding guidelines that affect the reimbursement rate for health systems, which have the tendency to change every year. Outsourced medical coders and billers, especially those who are certified by accredited organizations, have extensive and current knowledge of these codes given that they have to undergo an annual recertification exam to keep their credentials. This is especially useful in the process of improving clinical documentation.
- They submit accurate claims that improve revenue
Given that your RCM team are experts on diagnosis and procedure codes, you are assured that they are to make accurate claims submission that can positively impact revenue cycle. It has been proven that through CDI, revenue can be maximized. To support this, a 2016 Black Book Market Research survey found that nearly 90 percent of hospitals that used CDI solutions earned at least $1.5 million more in healthcare revenue and claims reimbursement.
RevCyle Intelligence, a leading online resource for the latest news and product information about the healthcare revenue cycle, claims reimbursement, and medical billing for providers, also reported that the Summit Healthcare Regional Medical Center in Arizona achieved a 20 percent increase in its case mix index after implementing a CDI program. Altogether, the case mix index improvement resulted in nearly $560,000 in additional revenue in less than a year.
- They allow physicians to focus on patient care
A 2016 AMA study reports that only 27% of their work time is spent on the patient, while 49% is consumed just for EHR documentation. In addition to more time being spent on records alone, they input an additional average of two hours after their work time for EHR data entry. Doctors spend more time inputting the information rather than observing the proper approach and discussing the treatment with the patients.
- They are certified with data privacy compliance
Because clinical documentation is often scanned into an electronic system and often interactive and viewed by simultaneously different healthcare providers, it is vital that patient’s records are kept safe and secured.
Although a patient’s record and chart belongs to the facility or healthcare organization, according to the Office of the National Coordinator for Health Information Technology the health record is “not just a collection of data that you are guarding—it’s a life”. Hence, there are three major ethical priorities for electronic health records: privacy and confidentiality, security, and data integrity and availability.
A great team of RCM are often HIPAA and DPA20212 compliant because they value privacy and confidentiality and understand that patient information should be released to others only with the patient’s permission or as allowed by law despite having all access to these records for the clinical documentation process.
With an outsourced team of RCM experts, clinical physicians will have more time in their hands to spend on patient interaction rather than on EHR and clinical documentation. Your RCM team can also work remotely with the following workout results:
- 95% coding, billing and documentation accuracy
- 1 hour turnaround time
- Improved denial management rate
- ISO 27001 and 9001, GDPR, HIPAA and DPA-20212 compliant
The right outsourcing partner not only ensure building a great and high-performing RCM team mentioned above but also ensure:
- Operational savings of up to 70%
- Clinical Documentation Improvement (CDI) and efficient process
- Information Security
- Maximize revenue
Partnership with Infinit-O
Infinit-O’s mission is to create endless opportunities for your company to realize its full potential.
Infinit-O Key Benefits:
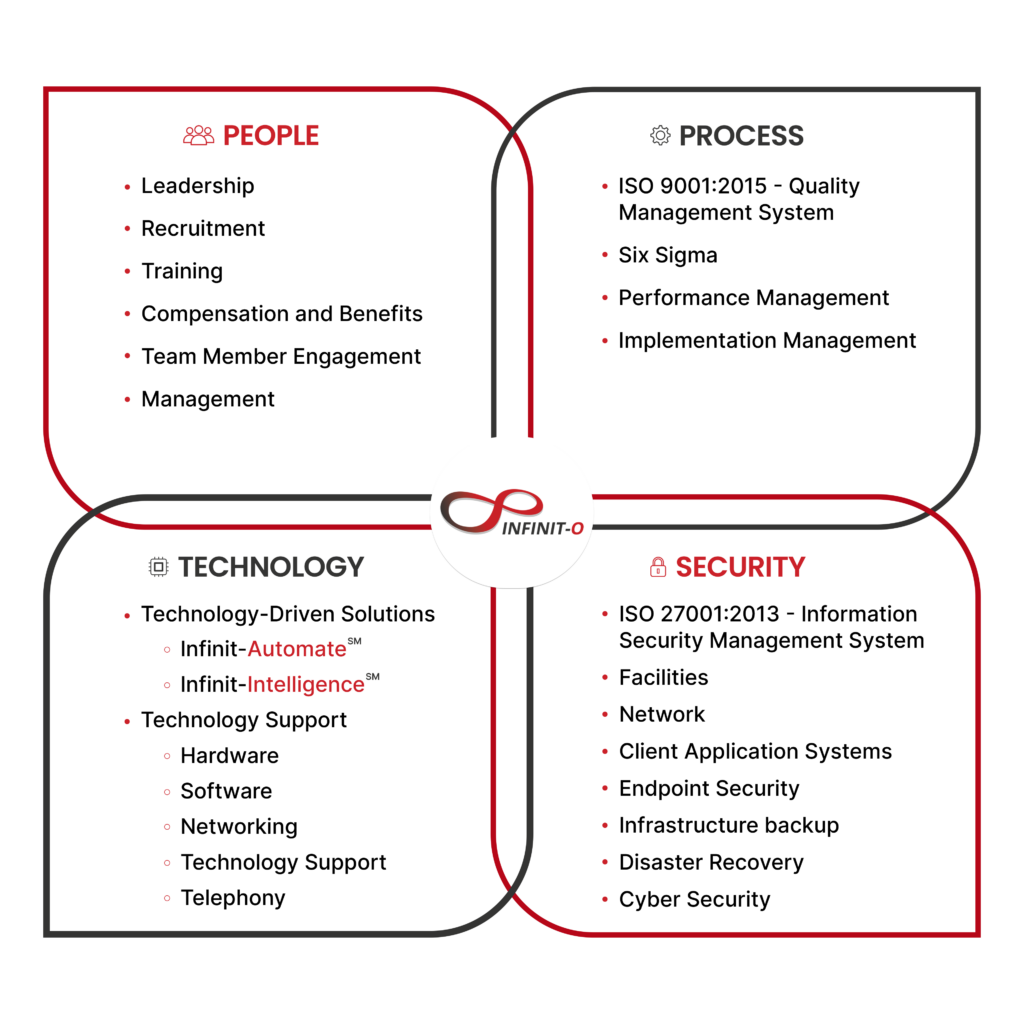
We can build you a great, high-performance Revenue Cycle Management team composed of:
Patient Support Services
- Patient Concierge Specialist
- Insurance Verification Specialist
- Collections Specialist
- A/R Specialist
Provider Management Services
- Medical Coders
- Medical Billers
- Claims Processors
- Enrollment Processors
- Denial Management Specialist
Health Analytics and Risk Management Services
- Healthcare Analyst
Others
Let’s work together to build a great RCM Team.
Start small. Exceed expectations. Think infinitely. Think Infinit-O.







This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.